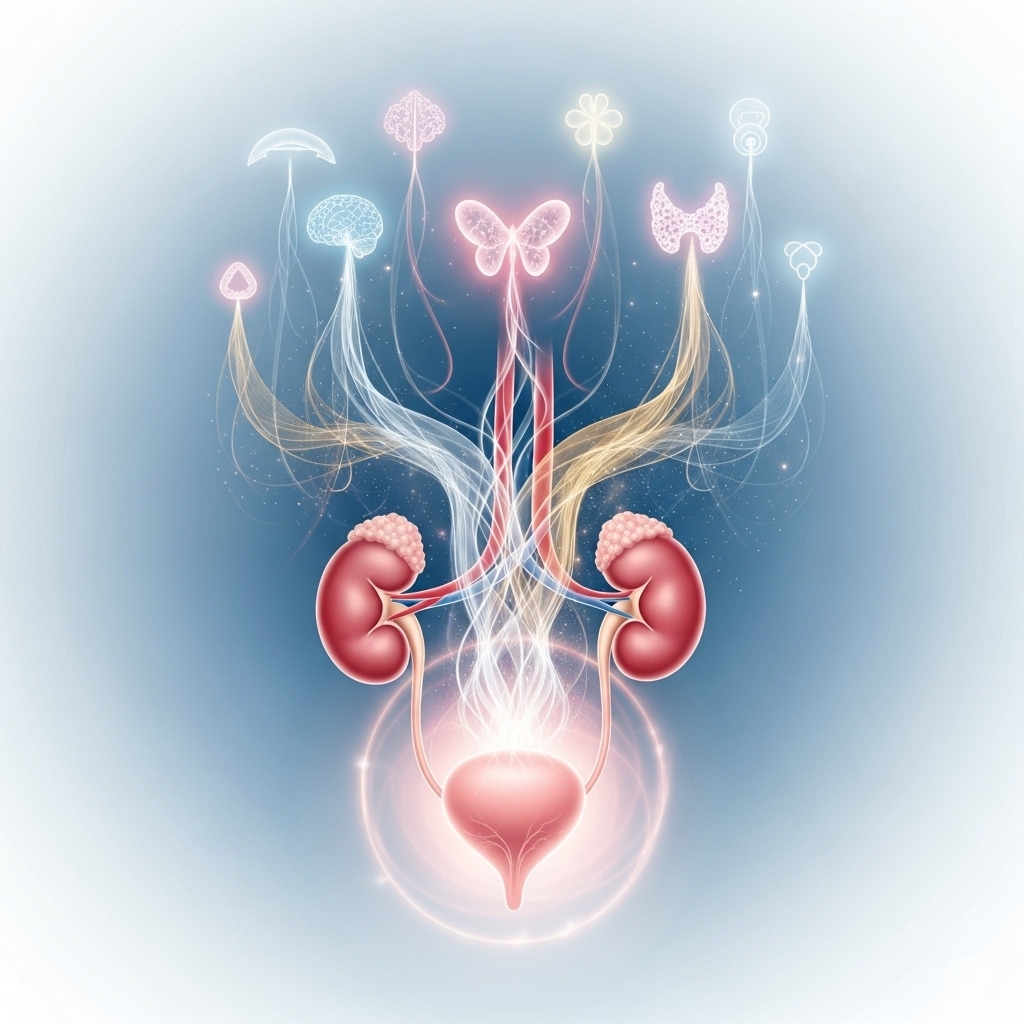
When we think about our urinary system, we often focus on the kidneys and bladder, but there’s a powerful and often overlooked player in their function: hormones. These chemical messengers influence nearly every system in your body, and the urinary tract is no exception. A delicate balance of hormones is crucial for healthy bladder and kidney function, and when this balance is disrupted, it can lead to a host of urological issues.
Estrogen: The Guardian of the Female Urinary Tract
Estrogen plays a pivotal role in maintaining the health of the female urinary system. It helps keep the tissues of the urethra, bladder, and pelvic floor strong and elastic.
- How it works: Estrogen receptors are found throughout the urinary tract. By binding to these receptors, estrogen helps maintain a healthy blood supply and the thickness of the urethral lining. This is essential for a tight urethral seal, which helps prevent involuntary urine leakage.
- When levels drop: As women age, especially during and after menopause, estrogen levels decline. This can lead to a thinning and weakening of the urethral and bladder tissues, often resulting in symptoms like stress incontinence (leakage when coughing, sneezing, or exercising) and urinary urgency. This is a key reason why hormone replacement therapy (HRT) or topical estrogen creams are sometimes used to treat menopausal-related urinary symptoms.
Testosterone: More Than Just a Male Hormone
While typically associated with male characteristics, testosterone also has a significant impact on the urinary system in both sexes.
- How it works: In men, testosterone helps maintain prostate health. An enlarged prostate (benign prostatic hyperplasia or BPH) can put pressure on the urethra and cause urinary symptoms. Testosterone also plays a role in bladder muscle function.
- When levels are low: Low testosterone levels (hypogonadism) have been linked to an increased risk of urinary tract infections and an overactive bladder in men. In women, low testosterone can contribute to a decline in muscle mass, including in the pelvic floor, which can worsen incontinence issues.
Thyroid Hormones: The Regulator of Kidney Function
Your thyroid gland, a small butterfly-shaped gland in your neck, produces hormones that regulate your metabolism. But these hormones also have a direct impact on your kidneys.
- How they work: Thyroid hormones (T3 and T4) influence the kidneys’ filtration rate and blood flow. A healthy thyroid helps the kidneys efficiently filter waste products from the blood and regulate fluid balance.
- When levels are imbalanced: Both an underactive thyroid (hypothyroidism) and an overactive thyroid (hyperthyroidism) can cause problems.
- Hypothyroidism can lead to a reduced glomerular filtration rate (GFR), which is a measure of kidney function. This can cause fluid retention and swelling.
- Hyperthyroidism can increase the GFR and lead to increased urination and thirst. In some cases, it can also cause kidney stones by altering calcium metabolism.
The Big Picture: Why this Connection Matters
Understanding the link between hormones and your urinary system is crucial for effective diagnosis and treatment. Urinary symptoms aren’t always a sign of a bladder or kidney disease; they can be a symptom of a broader hormonal imbalance.
If you’re experiencing persistent or unexplained urinary issues, it’s important to talk to your Urologist. They may recommend testing your hormone levels as part of a comprehensive evaluation. By addressing the root cause, whether it’s an estrogen deficiency, a thyroid issue, or another hormonal imbalance, you can find lasting relief and improve your overall health.