Pheochromocytoma
Adrenal Medulla Tumor: Pheochromocytoma
Pheochromocytoma is one of the essential adrenal tumors because, if left untreated can result in an uncontrolled hypertensive crisis and can be lethal. They secrete a hormone known as adrenaline/ noradrenaline and metanephrine, which maintains the body’s blood pressure by acting on the blood vessels, resulting in their contraction and keeping the body’s fluid equilibrium. Very high levels of these hormones can lead to an unchecked hypertensive crisis, which can be detrimental to one’s health or life. They are usually not cancerous but may be associated with many other thyroid and pancreas tumors.
What happens under normal conditions?
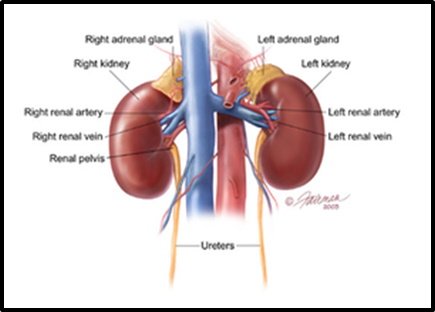
Adrenal glands are a pair of endocrine glands situated just above the kidney. They secrete many hormones, which maintain the body’s salt, sweet, and sex milieu. The cortex of the adrenal (outer half) secrets aldosterone and cortisol, which supports the body’s equilibrium of salt (electrolyte), glucose, and fluid—the medulla (inner half) secrets metanephrines, which maintain the body’s blood pressure.
Who is at risk for pheochromocytoma?
Pheochromocytoma can be associated with 1% of the young hypertensive patient, which can be corrected surgically. The incidence is the same in males and females and can be seen at any age but is most commonly seen in 20-40 yrs of age. One-third of the patients can present with tumors of other organs such as the thyroid, parathyroid or pancreas. This syndromic presentation is more common in children and includes multiple endocrine neoplasia type 2, Von Hipple-Lindau syndrome, neurofibromatosis and hereditary paraganglioma syndrome.
What are the symptoms of pheochromocytoma?
The classic triad of pheochromocytoma is headache, profuse sweating and palpitations. 15-20% of patients can have normal blood pressure or episodic rise in blood pressure. Other symptoms include anxiety, chest pain, abdominal pain, fatigue, weight loss, vision problems, the feeling of impending doom, panic attacks and seizures.
Hypertensive episodes can be triggered by trivial physical, emotional or pharmacological stimuli, including bending over, pressure on the abdomen, fear, tobacco, histamine and glucagon, or foods rich in tyramine (e.g., beer, wine and cheese).
Who should be examined for pheochromocytoma?
Patients with the following criteria should be screened for Hypertension:
- Uncontrolled Hypertension
- More than three medications required to control the blood pressure
- Early-onset of Hypertension.
- Patients with severe headaches, excessive sweating, palpitation, anxiety, nervousness, pain in the lower chest or upper abdomen, nausea, weight loss or intolerance to heat
How is pheochromocytoma diagnosed?
Once pheochromocytoma is suspected, 24 hour urinary VMA/ Metanephrine and serum metanephrine are done. To lateralize or locate the tumor, a CT scan or MRI. In an inpatient with extra-adrenal pheochromocytoma or recurrent or multiple pheochromocytomas, a meta-iodobenzylguanidine (MIBG) scanning or DOTA pet Scan is done.
How is pheochromocytoma treated?
Laparoscopic / Robotic surgical removal of the tumor is the standard treatment for pheochromocytoma if safe and feasible. Before the surgery patient is prepared to prevent any hypertensive crisis intraoperative by giving some medications, the preparation may take up to 2 weeks and may require hospitalization. Once the surgeon and the endocrinologist are satisfied that the patient is adequately prepared for the surgery, the patient is scheduled for tumor removal.
What can be expected after treatment for pheochromocytoma?
Persistent Hypertension can be present in about 25% of patients after removing pheochromocytoma. This is because of the pathophysiological changes because of prolonged ter hypertension. The patient needs to be under long-term follow-up as recurrent or metastatic diseases are known. The five-year survival rate after removing benign pheochromocytoma is around 84 to 96 percent.
