Radical cystectomy is a major surgical procedure often recommended for patients diagnosed with bladder cancer, particularly those with muscle-invasive bladder cancer (MIBC) or high-risk non-muscle invasive bladder cancer (NMIBC) that has not responded to other treatments. The procedure involves the removal of the entire bladder, and in some cases, nearby organs may also be removed to prevent the spread of cancer.
What is Radical Cystectomy?
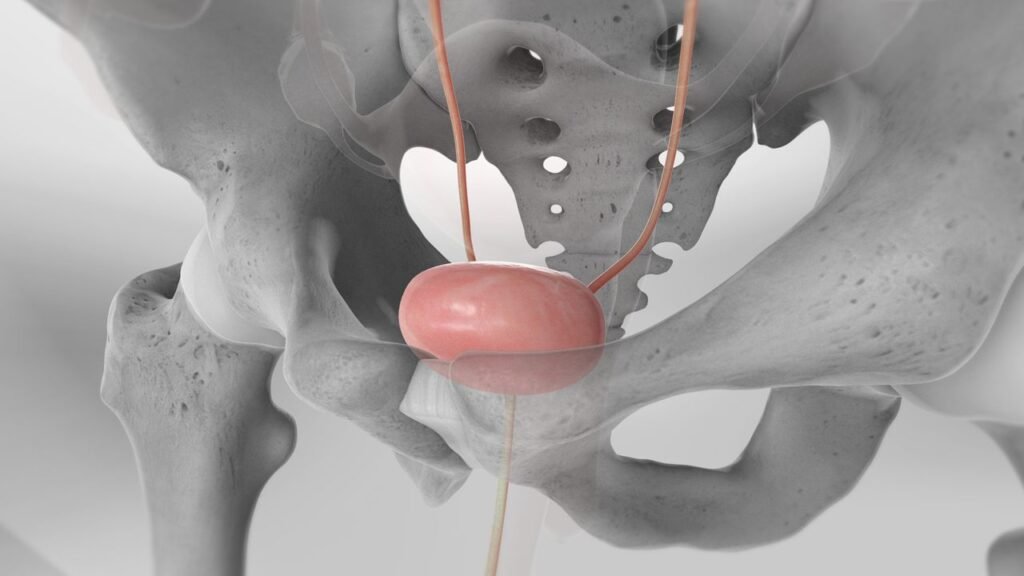
Radical cystectomy is the surgical removal of the urinary bladder. In men, this may also involve the removal of the prostate and seminal vesicles. In women, the uterus, ovaries, fallopian tubes, and part of the vaginal wall might be removed. The primary goal is to eliminate cancer from the body when it has advanced beyond the superficial layers of the bladder.
The surgery is usually combined with the creation of a new way to store and expel urine, as the bladder is no longer available to perform this function.
Indications for Radical Cystectomy
Radical cystectomy is most commonly performed for:
- Muscle-Invasive Bladder Cancer (MIBC): When bladder cancer invades the muscular layer of the bladder wall, radical cystectomy is often the most effective treatment to prevent cancer spread.
- Recurrent High-Risk Non-Muscle Invasive Bladder Cancer (NMIBC): In cases where cancer repeatedly returns after less invasive treatments like transurethral resection (TURBT) and intravesical therapy, radical cystectomy may be necessary.
- Bladder Cancer with Metastatic Potential: If cancer is found to be aggressive and has a high risk of spreading to other parts of the body, cystectomy can help in reducing metastasis.
The Procedure
Radical cystectomy is performed under general anesthesia, and the surgery can take several hours. During the procedure:
- Bladder Removal: The surgeon will make an incision to access the bladder and remove it along with any nearby organs that may harbor cancer cells.
- Urinary Diversion: Since the bladder is removed, the surgeon creates an alternative route for urine storage and elimination. This is called urinary diversion, and there are three main types:
- Ileal Conduit: A portion of the small intestine is used to create a conduit for urine to flow from the kidneys to a stoma (an opening on the abdomen), where it collects in a bag outside the body.
- Neobladder: A new bladder is created from a segment of the intestine, which allows for near-normal urination.
- Continent Urinary Reservoir: A pouch is made internally from the intestine, allowing patients to manually drain urine through a stoma using a catheter.
Recovery and Postoperative Care
Radical cystectomy is a complex surgery, and recovery can take several weeks or months. Patients usually spend 7-10 days in the hospital after surgery. Key aspects of recovery include:
- Pain Management: Patients may experience discomfort around the surgical site, which can be managed with prescribed pain medication.
- Mobility: Early movement and walking are encouraged to prevent complications such as blood clots and pneumonia.
- Diet: Gradually resuming a normal diet is common as the gastrointestinal tract adjusts after the surgery.
- Catheter Care: For patients with urinary diversion, understanding how to care for the stoma or catheter is crucial to avoid infections and complications.
Risks and Complications
Like any major surgery, radical cystectomy carries certain risks, including:
- Infection: Since urinary diversion involves handling the intestines and creating a stoma or catheter, the risk of infection is relatively high.
- Bleeding: Blood loss during and after surgery can occur.
- Blood Clots: Extended immobility after surgery can increase the risk of developing clots in the legs or lungs.
- Incontinence or Urinary Issues: Patients with neobladders or continent reservoirs may have issues with urine control.
- Sexual Dysfunction: Radical cystectomy can affect sexual function, especially if reproductive organs are removed. Nerve-sparing techniques are sometimes used to preserve sexual function, but this is not always possible.
Life After Radical Cystectomy
Adjusting to life after radical cystectomy can be challenging for many patients. Depending on the type of urinary diversion performed, there may be changes in body image, daily routines, and overall lifestyle. Support from healthcare professionals, counselors, and patient support groups can be invaluable during this transition.
For patients with ileal conduits, learning to care for the stoma and manage the external urine bag is essential. With time, many individuals can return to their normal activities, though some adjustments may be needed. Those with neobladders or continent reservoirs may need to retrain their bodies to empty urine, which can take several weeks.
Prognosis and Survival Rates
The success of radical cystectomy in treating bladder cancer depends on the stage and aggressiveness of the disease at the time of surgery. For early-stage bladder cancer that has not spread, radical cystectomy can be curative. For more advanced cases, the surgery can prolong survival and improve the quality of life by removing the cancerous tissue.
Long-term follow-up care is essential, including regular monitoring for recurrence, imaging tests, and urine tests to ensure the patient remains cancer-free.
Conclusion
Radical cystectomy is a life-saving procedure for patients with advanced bladder cancer. While it involves significant lifestyle changes, modern surgical techniques and postoperative care can greatly improve outcomes and quality of life for patients. For those facing this diagnosis, understanding the procedure, recovery, and potential complications can help in making informed decisions about their health and future.